Blog
How Optimized Testosterone Will Transform Your Life

The physiology of testosterone in the body
Let’s first talk about what testosterone is, what it does, and how it works. Testosterone is a hormone produced by the body that is needed for normal function in both males and females. It has a dominant role in males and its primary functions include:
Sexual differentiation: the development of sexual organs, such as the external genitalia and prostate.
Sexual characteristics: the development of masculine features, such as male hair patterns, voice deepening, muscle growth, and red blood cell production.
Spermatogenesis: the production of sperm in Leydig cells located inside the testes.
Fertility: the capability to produce offspring through reproduction.
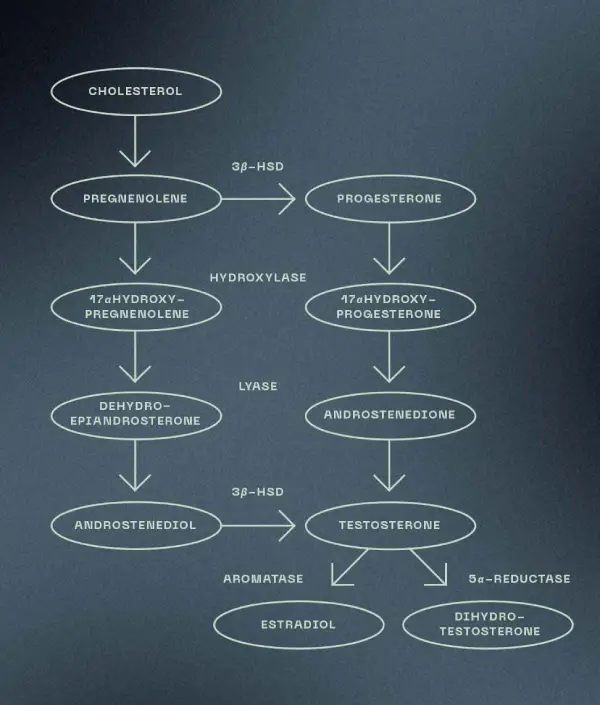
In males, testosterone is made inside of the testes (and androgens, male hormones that can be converted into testosterone, are made in the adrenal glands) from cholesterol. The pathway involves several enzymes and intermediates:
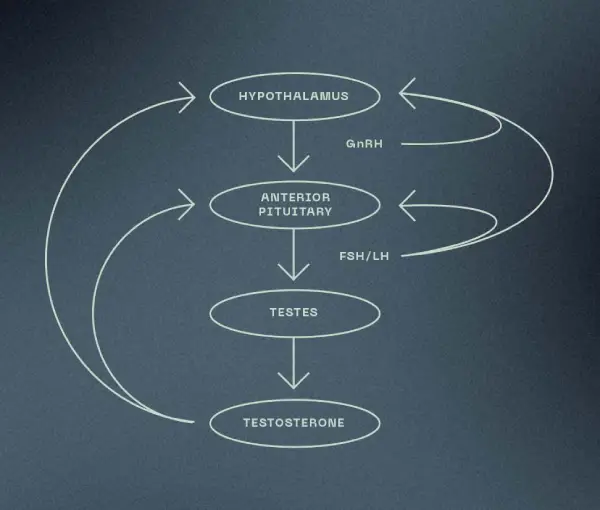
The production of testosterone is regulated by a cascade of signals between the brain and the testes. The hypothalamus (located inside the brain) monitors the amount of testosterone in the blood. If it senses that more testosterone is needed, it releases gonadotropin-releasing hormone (GnRH), which acts on the pituitary (located inside the brain) to release luteinizing hormone (LH) and follicle stimulating hormones (FSH). LH is responsible for stimulating the production of testosterone and FSH is responsible for stimulating the production of sperm. Once there is enough or too much testosterone in the blood, the hypothalamus will suppress the release of GnRH and FSH/LH, which inhibits the entire pathway and slows down testosterone production to decrease or maintain blood levels.
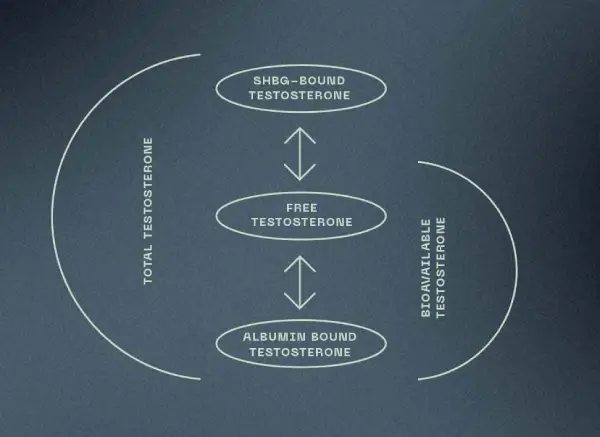
Once made, testosterone is released into the bloodstream where most of it travels bound to a protein (sex hormone binding globulin or albumin) and a small amount of it travels in free form. When testosterone is bound to SHBG, it is not available for use but serves rather as a surplus in the body. When testosterone is bound to albumin or in its free form, it is available for use (termed bioavailable testosterone) and can exert its powerful anabolic (building) and androgenic (masculine) effects on tissues such as the testes, bone, muscle, and prostate gland).
Benefits of Optimized Testosterone
Now that we know testosterone’s story, let’s cut to the chase: men feel their best when their testosterone is at an optimal level. Why, you might wonder? Because testosterone has a very strong influence on the male body. A man with optimal testosterone will experience beneficial effects on:
Body fat
Muscle mass
Bone density
Hair growth
Heart
Brain (memory, concentration)
Prostate
Metabolic health (blood sugar, lipids, body composition)
Red blood cell production
Stem cell production
Motivation
Mood
Energy
Physical performance
Physical recovery
Inflammation
Sexual activity/confidence
Libido
Wellbeing
On the other hand, a man with low testosterone may experience a range of negative signs, symptoms, and complications such as:
Low sex drive
Erectile dysfunction
Decreased sense of wellbeing
Decreased motivation
Depression, irritability, moodiness
Difficulty with concentration and memory
Fatigue
Loss of muscle mass
Decreased hemoglobin, mild anemia
Decreased body hair
Osteoporosis (thinning of bones)
Gynecomastia (breast development)
Infertility
Increased risk of diabetes and metabolic syndrome
Increased risk of Alzheimer disease
Associated with increased death from heart disease
The importance of optimized testosterone
All in all, optimized testosterone gives men the potential to live at max capacity, allowing them to flourish in their business, social, and personal lives. The problem is that most men’s testosterone levels are not at optimal levels and the conventionally defined normal range of testosterone is far from optimal.
The medical term for testosterone deficiency is male hypogonadism, which affects almost 40% of men aged 45 and older (likely underestimated and underreported). Testosterone deficiency is a well-established, significant medical condition that negatively affects male sexuality, reproduction, general health, and quality of life (IFM).
There are many factors that affect testosterone levels and cause or contribute to deficiency or insufficiency states, including genetic disorders, surgery, trauma, or certain diseases. However, the majority of hypogonadism (up to 89%) is not accounted for by these classic causes.
Factors of modern-day likely account for the majority of cases. Poor lifestyle, chronic stress, inflammation, and constant exposure to endocrine-disruptors and environmental toxins interfere with testosterone production and impede the endocrine system overall.
For example, exposure to phthalates (chemicals in plastics and personal care products) block normal testosterone production and ingestion of pesticides (chemicals used in farming to kill pests) and bisphenol A (BPA, a chemical found in plastic) reduces sperm count.
Low testosterone levels can make men physically weaker and softer as well as mentally depressed and uninterested in sex. Over time, these men lose their vitality. Unfortunately, these effects are normalized and accepted as a side effect of aging.
Testosterone levels do naturally decline with age, starting after age 30 and continuing at a rate of 1% per year throughout the rest of life. However, there is plenty that can be done to minimize the decline and keep levels in optimal range.
Interestingly, age-related testosterone decline may be a result of comorbidities that increase with age, rather than age itself – these include depression, elevated BMI, metabolic syndrome/type II diabetes, smoking, chronic disease, marital status, stress, and sleep (IFM).
In summary, if you want to attain or maintain your ideal physique, supreme cognition, healthy sexual/intimate relationships, ample ability to reproduce, and overall vigor, optimized testosterone levels are essential.
How to optimize testosterone levels
Bloodwork
In addition to a detailed history and physical exam, comprehensive bloodwork analysis is an important piece of assessment and treatment of low testosterone. Bloodwork can be used to diagnose deficient or insufficient testosterone and help identify the root cause. It is also necessary for monitoring and tailoring treatment. The standard normal range of total testosterone in the blood is generally 300 to 1000 ng/dL. Optimal levels of testosterone (the level at which a man feels his best) will vary greatly from man to man, which is why it is important to work with an ND at LIVV to monitor levels and help you find your sweet spot. Testosterone is typically measured in the morning between 7-10 am because this is when testosterone levels are at their peak in the body. Testosterone levels can be influenced by factors such as body mass index (BMI), nutrition, alcohol consumption, medication use (such as opioids for pain), age, illness, and certain diseases. Other biomarkers, such as SHBG, will be measured and additional testing may be needed with abnormal results.
Nutrition & Lifestyle
As always, a healthy diet and lifestyle are crucial for optimizing testosterone. Here are some of the most important elements:
Quality sleep: one study showed that getting only 5 hours of sleep per night decreased testosterone levels by 10-15%. GnRH pulses are regulated during sleep.
Stress management: cortisol and testosterone have an inverse relationship. Stress reduces testosterone due to its effects on the hypothalamic-pituitary-adrenal (HPA) axis in response to stress.
Weight management: obesity and insulin resistance – and their accompanying inflammation – are strongly associated with low testosterone. Excess fat increases the conversion of testosterone to estrogen.
Regular exercise: strength training at moderate and high intensities maximizes testosterone levels and protects against diseases of aging.
Good nutrition: vitamin A, vitamin D, zinc, and selenium are important for androgens and sperm production. Adequate protein and essential fatty acids are important for keeping SHBG in check.
Detoxification support: such as detoxification of heavy metal toxicity (e.g., cadmium) and supporting elimination of excess hormones.
Other: avoiding excessive use of alcohol and drugs, treatment of other hormone imbalances (e.g., cortisol, thyroid, estrogen).
You ND will be able to discuss each of these areas in much more depth. NDs are experts at creating individual lifestyle plans and incorporating biohacking techniques to optimize testosterone.
Natural Testosterone Replacement Therapy
Natural hormone replacement therapy works to increase testosterone levels using different modalities such as herbal medicine, supplements (such as DHEA and pregnenolone), medications that increase endogenous production (such as HCG and Clomiphene), peptide therapy that can support testosterone production, or testosterone replacement (such as injections or gels). Depending on your health condition and bloodwork results, the course of treatment may vary. Your ND will cover all the bases (safety, side effects, etc.) with you so that you feel comfortable with the treatment options that best suit you – call today to book your consultation!
Written by Jordan Valdez, RDN
References
Book:
The Testosterone Optimization Therapy Bible by Jay Campbell
Research:
Nassar GN, Leslie SW. Physiology, Testosterone. [Updated 2021 Jan 9]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK526128/
University of Chicago Medical Center. (2011, June 1). Sleep loss dramatically lowers testosterone in healthy young men. ScienceDaily. Retrieved January 1, 2022 from www.sciencedaily.com/releases/2011/05/110531162142.htm
Website:
https://my.clevelandclinic.org/health/diseases/15603-low-testosterone-male-hypogonadism
https://themenshealthclinic.co.uk/stress-testosterone/